Learn about the role, importance, skills, responsibilities, and challenges of an Insurance Verification Specialist. Find out what it takes to excel in this career.
Role of an Insurance Verification Specialist
Contents
An insurance verification specialist plays a crucial role in the healthcare industry, ensuring that patients have the necessary coverage for medical services. Their primary responsibility is to verify the patient’s insurance information, including coverage levels, co-pays, deductibles, and any pre-authorization requirements. This information is essential for healthcare providers to accurately bill patients and insurance companies for services rendered.
Additionally, insurance verification specialists also communicate with insurance companies to confirm the validity of coverage and resolve any discrepancies. They may also assist patients in understanding their insurance benefits and provide guidance on how to navigate the complex insurance process.
Furthermore, these specialists often work closely with billing and coding professionals to ensure that all information is accurate and up to date, reducing the risk of claim denials and delays in reimbursement. Their attention to detail and knowledge of insurance policies are critical in maintaining the financial health of healthcare providers.
Overall, the role of an insurance verification specialist is essential in facilitating the smooth operation of medical facilities and ensuring that patients receive the care they need without facing unnecessary financial burdens.
Importance of Insurance Verification Process
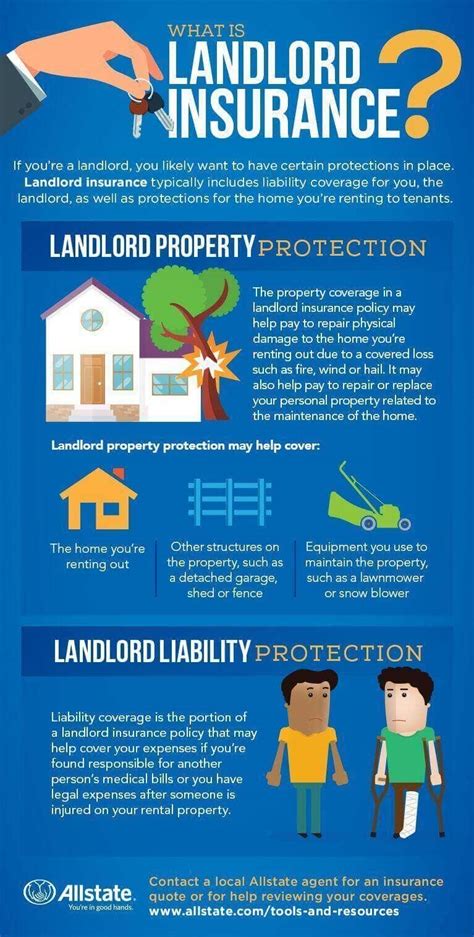
Insurance verification is a crucial process for healthcare providers and patients alike. It ensures that the medical services provided are covered by the patient’s insurance plan, reducing the risk of claim denials and out-of-pocket expenses for patients. By verifying insurance coverage upfront, healthcare facilities can avoid potential billing issues and delays in payment.
Moreover, insurance verification plays a vital role in maintaining accurate patient records and billing information. It helps in preventing errors and discrepancies that could lead to compliance issues or legal problems. This process also contributes to efficient revenue cycle management, as it allows healthcare providers to accurately estimate patient responsibility and collect payments upfront, reducing bad debt and improving cash flow.
Additionally, insurance verification ensures that patients receive the necessary pre-authorization for medical procedures and treatments. Without proper verification, patients may face unexpected obstacles in getting the care they need, leading to delays in treatment or unnecessary financial burden. Ultimately, the insurance verification process is essential for both healthcare providers and patients to ensure smooth and efficient healthcare delivery.
| Benefits of Insurance Verification |
|---|
| 1. Reduced claim denials and rejections |
| 2. Accurate patient billing and records |
| 3. Improved revenue cycle management |
| 4. Timely pre-authorization for medical care |
Overall, the importance of insurance verification cannot be overstated in the healthcare industry. It not only benefits healthcare facilities by streamlining the billing process and ensuring prompt payments, but also contributes to a positive patient experience by minimizing financial surprises and ensuring timely access to medical care.
Skills and Qualifications Required for the Job
Skills and Qualifications Required for the Job
Skills and Qualifications Required for the Job
Being an Insurance Verification Specialist requires a unique set of skills and qualifications to successfully perform the responsibilities of the job. First and foremost, a high school diploma or equivalent is typically required for this position. Additionally, having a detailed understanding of medical terminology, billing codes, and insurance policies is imperative for accurately verifying insurance coverage for patients.
Furthermore, strong communication and interpersonal skills are essential as the role involves constant interaction with both patients and insurance companies. The ability to effectively interpret and analyze insurance benefits and coverage details is crucial for making accurate determinations and providing the necessary information to patients.
In addition to these technical and interpersonal skills, attention to detail, organization, and time management are key qualifications for the job. An insurance verification specialist must be able to efficiently handle a high volume of insurance verification requests while adhering to strict deadlines and maintaining accurate records.
Lastly, proficiency in computer software and database management is often required for this role, as most insurance verification processes are performed electronically. Familiarity with medical billing software and Electronic Health Records (EHR) systems is highly beneficial for effectively navigating and documenting insurance information.
Responsibilities of an Insurance Verification Specialist
An Insurance Verification Specialist plays a crucial role in the healthcare industry, ensuring that patients’ insurance coverage is accurately verified before receiving any medical services. One of the primary responsibilities of an Insurance Verification Specialist is to review and verify insurance information provided by patients, including policy numbers, coverage limits, co-pays, deductibles, and any pre-authorization requirements.
Additionally, they are also responsible for communicating with insurance companies to obtain or confirm insurance coverage details, as well as to resolve any discrepancies or issues that may arise during the verification process. This involves collecting and documenting all necessary information accurately and thoroughly to ensure that the insurance claims process runs smoothly without any delays or rejections.
Furthermore, an Insurance Verification Specialist must stay updated on changes in insurance policies and procedures to ensure compliance with regulations and to provide accurate information to patients and healthcare providers. They may also be responsible for assisting patients with understanding their insurance coverage and addressing any questions or concerns they may have regarding billing or claims.
In order to excel in this role, strong attention to detail, organizational skills, and the ability to effectively communicate with insurance companies, patients, and healthcare staff are essential. Additionally, proficiency in medical terminology and insurance billing processes is also important for performing the responsibilities of an Insurance Verification Specialist effectively.
Challenges Faced in Insurance Verification
One of the biggest challenges faced in insurance verification is dealing with constantly changing regulations and policies. Insurance policies and coverage details are subject to frequent updates, which means insurance verification specialists must stay updated and knowledgeable about the latest changes in order to accurately verify insurance information for patients.
Another challenge is the high volume of insurance claims that insurance verification specialists have to process on a daily basis. This can be overwhelming and time-consuming, especially when dealing with incomplete or inaccurate patient information.
Additionally, insurance verification specialists often face challenges in navigating complex insurance systems and dealing with various insurance providers. Each insurance company may have different procedures and requirements, making it difficult to efficiently verify insurance coverage for patients.
Furthermore, the task of communicating with patients regarding their insurance coverage and potential issues can also be a challenge. It requires strong communication skills and the ability to effectively convey complex insurance information to patients in a clear and understandable manner.
In conclusion, the role of an insurance verification specialist comes with its fair share of challenges, from keeping up with ever-changing policies to managing a high volume of claims and navigating through complex insurance systems. However, with the right skills, qualifications, and determination, these challenges can be overcome to ensure accurate and efficient insurance verification for patients.